Heart disease remains the leading cause of death for both men and women in the United States. For many people, the first sign of trouble is a sudden heart attack. Fortunately, most heart disease is preventable – and often reversible – through daily habits that support cardiovascular health.
This guide summarizes evidence from preventive cardiology, lipidology, and lifestyle medicine to help you understand what protects (or harms) your arteries. The goal is to translate the science into practical steps you can use every day.
Key Takeaways
- Heart disease isn’t inevitable. Most of the factors that damage your arteries can be changed with the right habits.
- Not all numbers are created equal. Beyond LDL cholesterol, markers like apoB, blood pressure, A1c, and waist circumference are powerful predictors of cardiovascular risk.
- Food really matters. A heart-protective plate focused on vegetables, beans, and whole grains can lower cholesterol and inflammation naturally.
- Lifestyle is medicine. Movement, sleep quality, and stress management all directly influence your heart’s health—not just your weight.
- Small steps add up. You don’t need perfection; you need consistency.
Understanding What Really Drives Heart Disease
Heart attacks begin long before symptoms appear. The underlying process, atherosclerosis, develops when cholesterol-rich lipoproteins enter the artery wall and trigger inflammation. The latest American Heart Association cholesterol guidelines emphasize reducing LDL and other apoB-containing particles because these are the lipoproteins that initiate plaque formation.
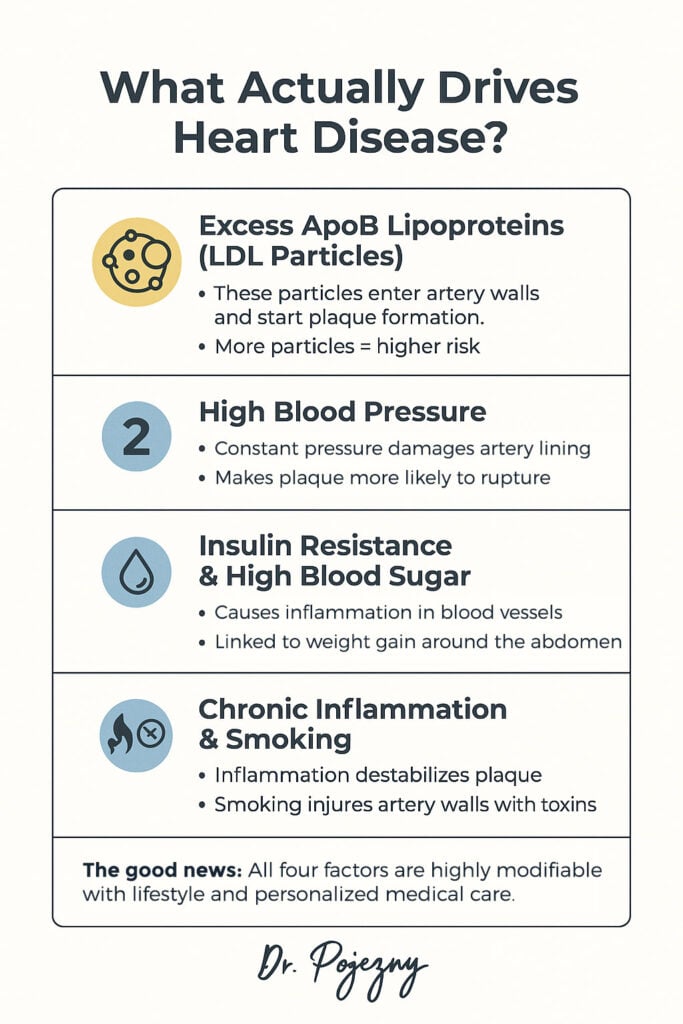
High blood pressure, insulin resistance, poor sleep, chronic inflammation, and smoking amplify this damage. Together, they create a stress environment that destabilizes plaque and increases the risk of heart attack.
The encouraging part: each of these biological drivers is highly modifiable with food, movement, stress control, and targeted medication when needed.
Food as a First-Line Therapy
A growing body of research consistently shows that diets rich in whole plant foods improve cholesterol, blood pressure, inflammation, and metabolic health. Clinical programs using plant-based diets have even documented regression of coronary artery disease, including the Lifestyle Heart Trial and the Esselstyn heart disease reversal study.

Whole plant foods are naturally high in fiber and antioxidants, both of which protect blood vessels. Colorful fruits and vegetables, especially berries and leafy greens, help reduce oxidative stress. Beans, lentils, whole grains, nuts, and seeds support healthier cholesterol and blood sugar levels.
Diets lower in saturated fat – such as plant-forward or plant-exclusive eating patterns – tend to reduce LDL cholesterol and apoB levels. For patients with diabetes or metabolic syndrome, low-fat plant-based diets have demonstrated significant improvements in blood sugar, weight, and insulin sensitivity, as shown in randomized trials published in Diabetes Care and the American Journal of Cardiology.
Resources that summarize this evidence for the public – such as the book How Not to Die – highlight how strongly whole foods impact long-term cardiovascular outcomes.
Weight, Metabolism, and the Heart
Excess abdominal fat increases inflammation, insulin resistance, and blood pressure. Improving metabolic health through sustainable changes—not crash diets—can significantly reduce cardiovascular strain.
Clinical trials have shown that emphasizing vegetables, beans, whole grains, and fruits helps with natural calorie control, because these foods are fiber-rich and low in calorie density. In people with type 2 diabetes, plant-based diets led to measurable improvements in blood sugar and cholesterol in controlled studies published in Diabetes Care.
Eating more of your calories earlier in the day may also improve metabolic outcomes, as the body handles glucose more efficiently in the morning than late at night.
Know the Numbers That Actually Matter
Traditional LDL cholesterol is important, but modern cardiology now places strong emphasis on apoB – the count of all atherogenic lipoproteins capable of entering the artery wall. ApoB and lipoprotein(a) (Lp(a)) testing are recommended in many adults, according to updated AHA/ACC guidelines.
Monitoring blood pressure, fasting glucose, A1c, and waist circumference also provides insight into cardiovascular risk. Lifestyle changes often improve all these markers at once.
When lifestyle alone isn’t enough, medications such as statins, ezetimibe, or PCSK9 inhibitors can meaningfully reduce risk. These therapies are strongly supported by the AHA/ACC Cholesterol Guideline Summary.
Movement as Medicine
Regular physical activity improves blood pressure, insulin sensitivity, circulation, and inflammation. The American Heart Association’s activity guidelines recommend 150–300 minutes of moderate exercise per week or 75–150 minutes of vigorous exercise. Even walking can significantly reduce cardiovascular mortality.
“Movement snacking” – brief walking breaks or gentle bodyweight exercises – can be as beneficial as longer sessions when added throughout the day.
The Underrated Pillars: Sleep, Stress, and Smoking Cessation
Sleep deprivation raises blood pressure, worsens insulin resistance, and increases inflammation. Large reviews (for example, those published in Sleep and Circulation) consistently show higher cardiovascular risk in adults who regularly sleep less than 6–7 hours.
Stress reduction through prayer, deep breathing, journaling, counseling, or meditation calms the sympathetic nervous system and protects the heart.
Smoking remains one of the most harmful modifiable risk factors. The U.S. Surgeon General’s 50-year report on smoking details how quitting at any age rapidly reduces cardiovascular risk. Medications and structured programs greatly improve success rates.
A Day in the Life of Heart-Protective Habits
A heart-healthy day might begin with oatmeal topped with berries, banana, flaxseed, and walnuts. Lunch may include a large salad with beans, greens, vegetables, and a vinegar-based dressing. A brief walk after meals improves blood sugar control.
Dinner might include a lentil stew, bean chili, quinoa bowls, or vegetable-heavy plates. An evening routine that protects sleep rounds out the day.
Lifestyle and Medication: A Combined Approach
Some patients can normalize cholesterol, blood pressure, and glucose with lifestyle changes alone. Others, especially those with genetic risks or existing heart disease – benefit from combining lifestyle therapy with medication. This balanced approach is supported throughout major prevention guidelines, including the 2018 Cholesterol Guidelines.
Food, movement, sleep, and stress reduction form the foundation. Medications build on that foundation when needed.
Taking the Next Step
Start by reviewing your latest labs, including cholesterol and blood sugar. Ask your doctor whether measuring apoB and Lp(a) could better clarify your risk. Gradually shift meals toward whole plant foods, add daily movement, protect your sleep, and seek support for smoking cessation if you need it.
Your heart responds quickly to positive change, and each small step moves you toward a longer, more vibrant life.






